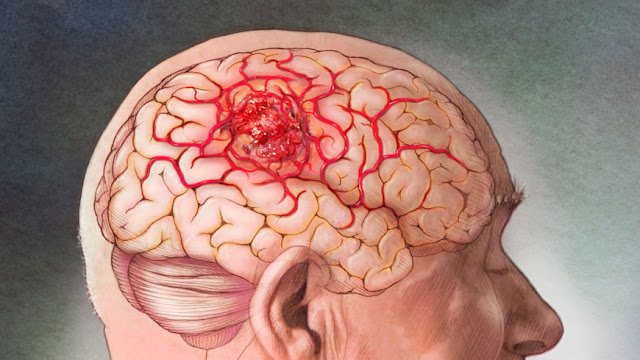
A cavernoma, also called cavernous angioma, is a vascular
malformation in the brain. The blood vessels are abnormally dilated and look
like "little caverns" (hence the name), and are clustered together in
the shape of a small sphere. Three symptoms are characteristic of a cavernoma:
a sudden neurological deficit, a seizure, or a slow neurological deterioration.
These are usually related to bleeding from the cavernoma, its growth, or
changes in the microcirculation. Its discovery is, more often than not, lucky,
and it generally requires a regular follow-up. You can treat this disease with
the help of telehealth psychiatry services.
Definition and Symptoms
What is Brain Cavernoma?
A cerebral cavernoma is a malformation of the brain's blood
system: the vessels are abnormally dilated. In the majority of cases, this
anomaly does not involve any symptoms. Sometimes neurological disorders
(headaches, blurred vision, etc.) are present.
The number of individuals with this malformation is
difficult to assess. In particular, because a cavernoma is often asymptomatic,
many patients are unaware that they have one. According to various studies on
the subject, the number of carriers of a cerebral cavernoma is estimated
between 1 in 200 and 1 in 1000.
A cavernoma affects men and women equally, regardless of
their origin. It generally demonstrates between the ages of 20 and 40 but can
also lead to symptoms in childhood or adolescence.
The exact origin of this vascular malformation is still
unclear. We only know that it is a local anomaly in the development of the
vessels. Indeed, a cavernoma consists of small vessels (capillaries) very
dilated, twisted, and grouped. A cavernoma looks like a ball of small,
intertwined vessels. Its size varies from some millimeters to several centimeters.
20% of cerebral cavernomas are familial forms. In other
words, the malformation is associated with a genetic anomaly that is passed on
from generation to generation. The genes involved in cerebral cavernoma are
CCM1, CCM2, and CCM3. These familial forms often result in the presence of
several cavernomas. They carry a greater risk of complications.
To know! We can
roughly think of genes as codes for producing proteins. These are essential
elements because they contribute to each cell's proper functioning and,
therefore, more generally of the body.
What Symptoms?
In the vast majority of cases, namely nearly 90%, the
cerebral cavernoma is asymptomatic and remains silent. It is then often
discovered by chance during an MRI (Magnetic Resonance Imaging) for another
health problem.
In the remaining 10% of cases, the cavernoma is the cause of
various symptoms. The first occurs between 20 and 40 years old. They can result
in epileptic seizures (up to 70% of cases), headaches, or other neurological
disorders (vision disturbance, sensitivity disorder in the limbs, etc.).
Symptoms vary a lot from patient to patient and depending on the number of
cavernomas, size, and location.
More rarely, some individuals may occasionally exhibit
non-neurological symptoms, including red spots on the skin and asymptomatic
malformations of the blood vessels in the retina. This type of symptom is more
likely to affect patients with the familial form of the disease.
When they exist, symptoms may be due either to the cavernoma
itself or to the bleeding caused. The walls of cavernomas are thin and fragile,
so they break easily, causing an effusion of blood, which can damage the
impacted brain structures. However, even in the incident of a rupture, the
bleeding is small. Thus, loss of consciousness or coma is very exceptional.
Also, an increasing size cavernoma can sometimes compress the brain areas
surrounding it and cause neurological disorders. Finally, epilepsy is linked to
the irritation of certain parts of the brain in contact with the cavernoma.
Diagnostic
Brain Imaging
(MRI)Magnetic resonance imaging of the brain is the gold
standard for the diagnosis of cerebral cavernomas. The gradient echo sequence
(T2 *) is the most sensitive for identifying cavernomas due to its high
sensitivity for detecting traces of bleeding in brain tissue. MRI also makes it
possible not only to make the diagnosis but also to date the hemorrhage,
monitor the evolution of the cavernoma (s) and highlight an associated venous
developmental anomaly.
A classification into four categories has been proposed. It
is based on MRI of the cavernoma (hyperintense, hypointense) on different
sequences (T1, T2, gradient echo). To each type corresponds information
concerning the characteristics of the cavernoma (type I: recent bleeding, type
II: heterogeneous lesions with bleeding and thrombosis of varying ages, type
III: old bleeding, type IV: aspect evoking a cavernoma in the process of the
constitution)
The follow-up studies of familial cavernomas have confirmed
the dynamic nature of these malformations in brain imaging. The evolution of
cavernomas can result in new lesions or changes in their characteristics
(particularly their size). The demonstration of endothelial proliferation at
the periphery of vascular cavities suggests that angiogenesis phenomena could
increase the volume of certain cavernomas.
Vessel Imaging
Cavernomas are not visualized with angiography techniques
(CT angiography, magnetic resonance angiography, or cerebral arteriography)
because the circulation within the "caverns" (cavities making up the
cavernoma) is done at low flow, and the vessels feeding the malformation. They
are very small sizes. Sometimes imaging of the brain vessels is necessary to
rule out another type of vascular malformation. This examination sometimes
reveals a developmental venous abnormality associated with the cavernoma.
Genetic Diagnosis
The identification of CCM genes today makes it technically
possible to screen these three genes in hospital practice. In the infinite
majority of cases, the mutations identified lead to a premature stop codon's
appearance or partial or complete deletion of one of the 3 CCM genes.
The screening sensitivity in a subject with familial
adenomatosis is approximately 94% (see above), while it is only 57% for a
sporadic case with multiple lesions.
Once the mutation has been identified in a patient, the
test's sensitivity reaches 100% for his relatives.
The decision to carry out a genetic test must be preceded by
a preliminary analysis of this test's real benefit, particularly in the case of
an asymptomatic subject. These tests' indication appears to be very variable
and varies in different situations (see next chapter).
What Evolution?
Among patients with asymptomatic single cerebral cavernoma,
a minority will take one day to present with neurological symptoms.
People who have
symptoms may either stabilize, or even regress, or worsen over time.
The evolution of a cavernoma depends mainly on its risk of
bleeding and its location in the brain. A cavernoma is not a precancerous
lesion, so there is no risk of cancerization or spread to the rest of the body
to worry about.
Comments
Post a Comment